When it comes to Orthopedic Medical Billing, many practices find themselves dealing with complex processes that involve nuanced rules and resolutions. This is especially true in Orthopedics, which covers musculoskeletal conditions affecting bones, joints, ligaments, and tendons. Ensuring accurate medical billing is critical to your practice's success, as costly mistakes can significantly affect your bottom line. At SitMD Medical Billing, we've seen firsthand how eliminating coding errors can lead to a healthy revenue cycle, allowing your orthopedic practice to focus more on patient care and grow your business with ease. It’s not just about completing the paperwork; it’s about ensuring your practice can scale faster and more efficiently.
Optimizing the revenue cycle is essential for every medical practice, especially in Orthopedics. Efficient management of orthopedic services ensures timely payments, reduces delays, and improves cash flow. Following billing and coding guidelines and maintaining accurate billing practices are key to reducing the risk of denied claims. Adhering to CPT codes and minimizing errors can create a smoother operation, contributing to the financial stability of your practice. At SitMD Medical Billing, we help you manage your income-derived resources and address billing concerns, allowing your practice to focus on what matters most—providing exceptional care to your patients while optimizing your overall revenue cycle.
Orthopedic billing complexities include coding variability, high denial rates, and insurance pre-authorizations, requiring precise documentation and proactive claim management.
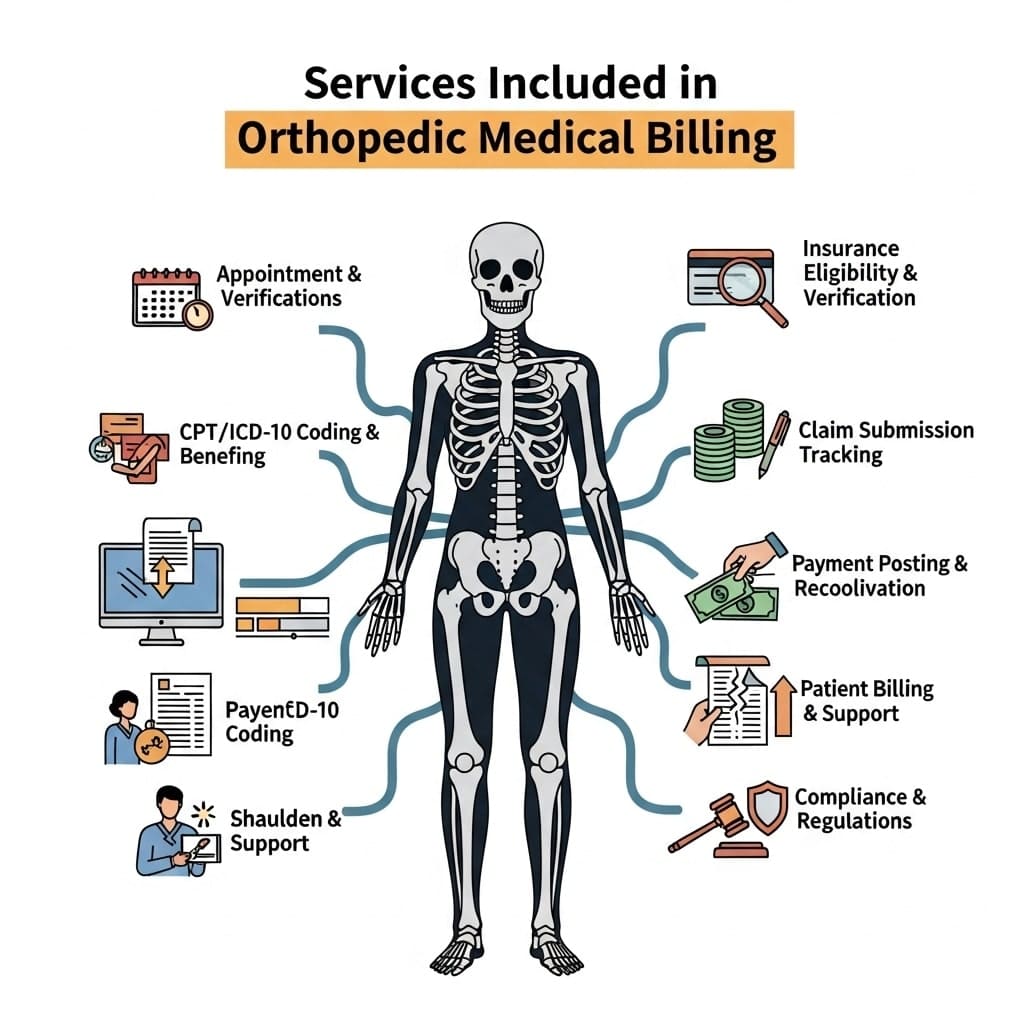
In orthopedic medical billing, accurately documenting all aspects of a patient’s visit is critical. From the initial entry of patient demographics to insurance eligibility verification, everything must be correctly logged for smooth claims submission. Documentation and coding of services and procedures performed during the visit are critical to ensuring maximum reimbursement. Timeliness is crucial; timely claims submission helps prevent delays and ensures that the healthcare provider gets paid for the services rendered.
Sometimes, claims are denied for various reasons. In these cases, reprocessing denied claims becomes a key part of the process. It involves reviewing the reasons behind the denial and resubmitting the claim with necessary corrections. This back-and-forth process is essential in maximizing revenue and ensuring that all services performed are compensated accurately. Effective management of this process ultimately ensures that orthopedic medical billing contributes to the practice’s financial health.
In orthopedic medical billing, errors can pose significant challenges, affecting both the efficiency of the healthcare practice and financial outcomes. One of the most common mistakes is incorrect or outdated coding. This occurs when CPT codes, diagnosis codes, and modifiers are not aligned with the procedures performed, leading to claim denials and underpayments.
Additionally, when services that should be bundled into one code are billed separately, known as unbundling, it can result in penalties and delayed reimbursements. Upcoding and down-coding—either overestimating or underestimating the complexity of a procedure—are also frequent errors that impact claim processing. Lack of specificity in coding, such as failing to provide the highest level of detail, can also lead to issues, especially in quality reporting.
Another issue often seen in orthopedic billing is related to administrative and documentation errors. Typos or missing details, such as remote patient information like date of birth or insurance numbers, can cause claims to be rejected. Inaccurate or incomplete medical necessity documentation, especially for procedures like joint replacements, which require proof of conservative treatments before approval, is another common mistake.
Moreover, failing to secure prior authorization or missing filing deadlines for claims often results in automatic denial. For practices that rely on timely reimbursement, this can mean significant delays and lost revenue. Finally, understanding the payer-specific rules for each insurance company is crucial. Not following these rules can result in delays or denials.
Furthermore, a lack of proper follow-up on denied claims, including failure to appeal them, often results in lost revenue. Poor communication among front desk staff, providers, and the billing department can also contribute to these problems, making it harder to stay on top of claims and ensure that all necessary information is included. These issues, if left unaddressed, can hinder the revenue cycle and ultimately impact the practice’s financial health.
In orthopedic practices, failing to properly verify a patient’s insurance eligibility can lead to serious issues. When coverage isn’t confirmed in advance, it increases financial risks and can lead to significant delays in claim processing. This can result in denied claims and higher patient bills, as the patient may be held responsible for expenses that should have been covered. It’s crucial for practices to verify insurance eligibility to prevent costly mistakes and improve the likelihood of smooth reimbursements.
In orthopedic billing, all patient demographic data must be entered correctly. Even the slightest error, like an incorrect date of birth or a misspelling, can cause problems. These small mistakes are often enough to trigger automatic denials from insurance companies, delaying payments and complicating the billing process. Ensuring accuracy in this step is vital for a smooth orthopedic billing process and timely reimbursements.
In orthopedic billing, ensuring correct documentation of each service and procedure is essential. Incomplete notes or missing reports can lead to inaccurate coding, resulting in denied claims and delayed maximum reimbursement. It’s important to use the right ICD, CPT, and modifier codes for proper billing.
For Example, Proper coding for fracture care, such as using Q codes for custom-made casts and braces, rather than for prefabricated ones, is vital. Keeping up with billing guidelines and changes is necessary for the staff to stay up to date and avoid costly errors.
In orthopedic billing, it’s crucial to submit claims promptly and ensure they are timely and accurate. Delayed claims drag out the process, increasing the risk of denials and the need to reprocess them. This not only prolongs revenue but also makes it harder to receive reimbursement on time. If the claim slips through the cracks, it could lead to lost revenue and affect the practice’s overall financial health. Eliminating delays in submission is key to reducing these risks and ensuring smoother cash flow.
Navigating chronic care management and ensuring compliant coding are vital steps to ensure your claims are submitted correctly and efficiently. It’s not just about submitting the right information—it’s about ensuring it complies with the relevant requirements set by CMS, AMA, and other governing bodies. By doing so, you help avoid costly fines and penalties from insurance companies.
Every claim document you submit must be scrutinized to comply with HIPAA regulations and the ever-evolving guidelines from federal and state authorities. If denials occur due to non-compliance, they can delay claim processing and disrupt your healthy revenue cycle. To verify compliance with these regulations, it’s crucial to ensure your coding is accurate, which, in turn, promotes faster claim processing.

Outsourcing your Orthopedic medical billing to experts can greatly reduce the frustration and financial stress your staff may face when handling complex coding and claims. With specialists like Coronis Health, your practice can significantly reduce denials and increase reimbursement. These experts ensure that every claim submission complies with changing regulations and meets the relevant requirements, reducing the risk of denied claims. This allows your practice to streamline its revenue cycle and focus more on patient care.
Working with Orthopedic billing consultants ensures quicker claim submissions, faster processing, and more time for your staff to focus on the patient. Not only do you benefit from KPI reports to track financial performance, but you also relieve your team of administrative burdens, allowing them to focus on what matters most: providing excellent patient care. With outsourcing, your practice can operate more smoothly, making the most of every opportunity to grow and succeed.
Choosing SitMD for your orthopedic billing needs means you get a team of experienced specialists and coders who stay up to date on the latest industry standards. Their expertise allows them to efficiently manage your coding and workflow, ensuring a high first-pass claim rate and reduced denial rate. This can significantly reduce A/R days and streamline your practice’s billing process, allowing you to focus more on patient care.
SitMD offers a proven solution to overcome common orthopedic billing challenges. Their team is well-versed in evolving industry standards and is committed to delivering benefits such as accurate claim submissions and faster processing. By partnering with SitMD, you ensure your billing process is in expert hands, leading to improved financial outcomes for your practice.
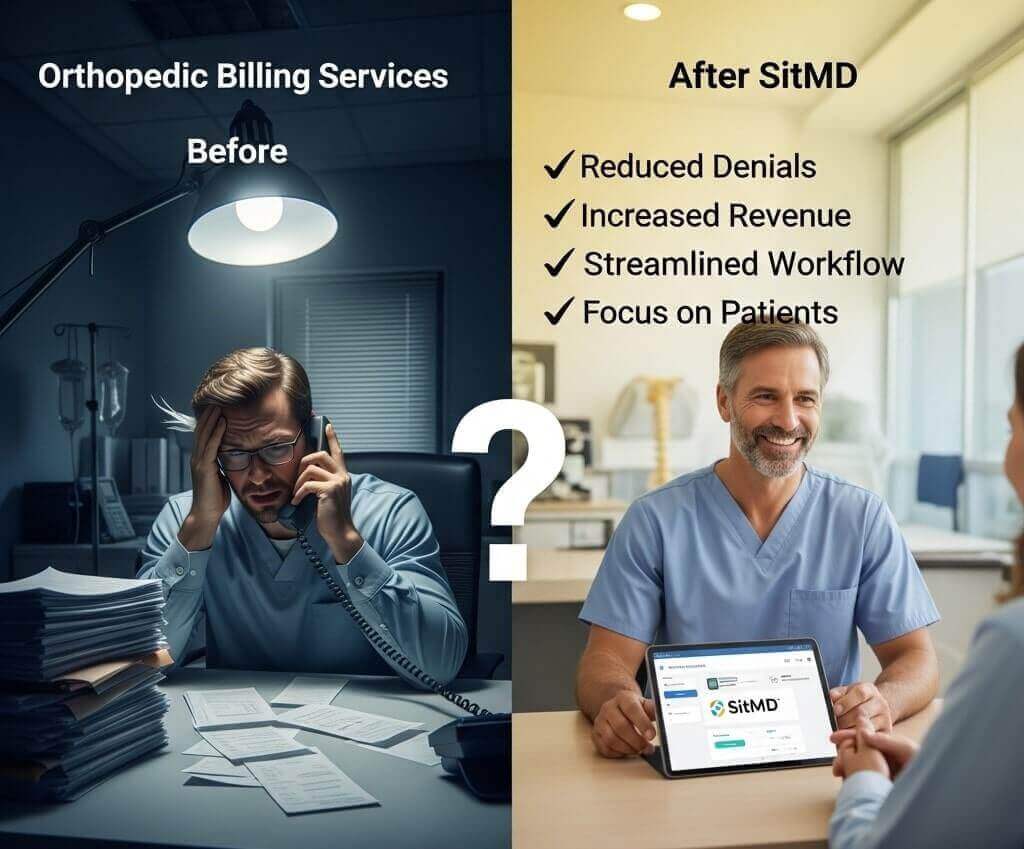
At SitMD, we understand that orthopedic medical billing comes with unique challenges that can lead to costly errors if not managed properly. By implementing best practices and staying up to date with the latest industry standards, we help our clients navigate these complexities.
Our coding professionals are experts at ensuring accuracy in ICD-10, CPT, and other billing codes, reducing the risk of denials and ensuring reimbursements are processed smoothly. We focus on eliminating errors such as overuse of laterality modifiers, incorrect T-codes, and missed parenthetical notes that can cause problems.
With SitMD, your practice can streamline its revenue cycle management to ensure claims are submitted the first time, leading to fewer denials and quicker payments. Our team works diligently to ensure every detail is covered, from diagnosis codes to documentation of symptoms and signs. By preventing these common errors, we help your orthopedic practice avoid disruptions and maintain financial stability.
Orthopedic medical billing presents unique complexities that require precise documentation and a strong understanding of services rendered during patient visits. Small errors, such as submitting insufficient information or failing to verify eligibility in time, can lead to denied claims.
These issues can disrupt your revenue cycle management, delay payment from the insurer, and even force your clinic into a financial bind. Having skilled coding staff is essential to navigating these challenges, ensuring that claims meet authorization requirements and align with the insurer’s preferences. By staying on top of deadlines, you can avoid denials and ensure that your practice is paid accurately and on time.
At SITMD, we specialize in reducing administrative burdens, increasing reimbursements, and ensuring compliance for orthopedic practices. Our dedicated billing professionals handle the complexities of medical billing, allowing you to focus on patient care while we optimize your revenue cycle.
The most common CPT code for orthopedic patients is 20610, which is used for major joint injections/aspirations. This code is often used for joint injections or aspirations to relieve pain. Other frequently used codes include 27447 for total knee arthroplasty and 27130 for hip replacement. For procedures like knee arthroscopy with meniscectomy, 29881 is commonly used, while 64721 applies to carpal tunnel release. Codes like 99202 and 99215 are used for evaluation and management, and 29827 is used for rotator cuff repair.
An orthopedic surgery coding cheat sheet is crucial for medical billing because it helps improve accuracy and ensures compliance with payer and government regulations. This cheat sheet provides coders with quick access to essential information, including CPT and ICD-10 codes, modifiers, and billing guidelines, to help them handle the complexity of orthopedic procedures correctly. By reducing the risk of denials, it ensures timely reimbursement and minimizes errors, making the billing process more efficient.
In orthopedics, there isn’t a single CPT code because each orthopedic procedure is assigned a specific code based on the service performed. For example, Evaluation and Management (E/M) codes like 99202 and 99205 are used for office visits with new patients. On the other hand, surgical procedures such as 27447 are used for specific treatments, such as total knee arthroplasty. These codes are categorized into different ranges to cover various orthopedic services and treatments.
In orthopedics, evaluation and treatment are coded using specific CPT codes. For Evaluation and Management (E/M), codes 99202 and 99205 are used for new patients, while 99212 and 99215 are used for established patients. Treatment codes vary by procedure type. For example, 27447 is used for knee arthroplasty, and 20610 applies to arthrocentesis of musculoskeletal joints and tissues. There are also codes for fracture care, spine procedures, and diagnostic imaging, which help to cover a range of orthopedic services.
If you’re struggling to keep up with the competitive healthcare landscape, it’s time to take action. Let your orthopedic practice not just survive but thrive by partnering with a dedicated billing specialist.
By hiring a professional, you can ensure your practice stays ahead with expert billing support and optimized revenue. Don’t wait—contact an orthopedic billing specialist today and give your practice the edge it deserves.
We deliver tailored billing solutions, ensuring accurate reimbursements, seamless operations, and compliance for practices across various Healthcare revenue cycle disciplines.




























Discover our expert anesthesia care for a pain-free and secure medical experience.
